Most women want safe contraception and therefore use hormonal contraceptives like the pill, the ring, or patch. When the pill was developed in the 1960s, the researchers wanted to mimic the natural cycle of the woman, which averaged 28 days (although wide variations are frequent and normal).
The break for a monthly bleed is not based on a biological need, but was introduced by the inventors of the pill for marketing purposes to imitate a ‘natural’ cycle, and thereby increase women’s acceptance of the pill, as well as facilitate approval by the FDA, the American health authority. It was feared that the FDA and women would probably reject the new pill if women were neither pregnant nor menstruating. This rationale is described by the inventor of the pill, biochemist Gregory Pincus, in his biography:
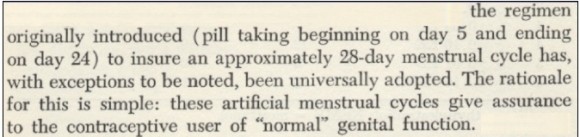
Source: Gregory Pincus, The control of Fertility, 1965, www.muvs.org
Read the exciting story about the invention of the pill: A forgotten revolution: muvs.org
Video: de.muvs.org
Are monthly bleeds with the pill important or can I do without?
Today’s pills are based on this same 28-day cycle. For example, the most commonly used pills contain 21 tablets in a blister pack, with instructions to take a tablet each day for 21 days, followed by a 7-day break, the “intake-free interval”. (Cycle: 21 days + 7 days = 28 days). Some pill packets come with 24 days of tablets and a break of 4 days. Other packets contain 4 or 7 inactive tablets (a placebo), so that women can just take a tablet every single day.
Women in the 1960s and many today still consider monthly menstruation to be natural, so the 21 + 7-day scheme is still the most frequently used. Since the pills are designed to induce artificial monthly bleeding – i.e., not a natural menstruation – it’s also called withdrawal or break bleeding. The withdrawal causes hormones level to drop over the 7-day break. The uterine lining, which has built up over the 21 days of taking the pills, is expelled and bleeding occurs. However, the bleeding is usually weaker than a real period and less painful.
From a medical perspective, the monthly bleeding is not necessary. Research and development over the last few decades have significantly reduced the hormonal dosage of modern pills. The future trend for the pill will be to omit monthly bleeding entirely, which is perceived by many women today as bothersome and unnecessary.
After consulting with your doctor, you can take the pill (single-phase preparations) without a break using the long cycle. After 6 months maximum, you should take a break for 4-7 days. This may trigger bleeding to expel the built-up uterine lining, but probably not heavier than a normal period. The long cycle reduces bleeding to twice a year if you take the pill for 6 months, or four times a year if you take it for 3 months.
Ask your doctor.
Also read this article: Menstruation – is it necessary? Part 1 Menstruation – is it necessary? Part 2
 Why Menstruation?
Why Menstruation? 